Both flowers and humans need sunlight, while one needs for photosynthesis, the later needs for production of Vitamin D. While women are more conscious about this, Indian men tend to overlook the requirement of Vitamin D and live with the symptoms before it starts troubling them. Max Muller has once quoted that “a flower cannot blossom without sunshine and a man cannot live without love”. In India, considering the reports of Vitamin deficiency in Indians, we can say for sure that even Indian men can’t blossom without sunshine.
The term “vitamin D” refers to compounds vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol). Vitamin D3 is produced in the skin on exposure to sunlight. Vitamin D3 is derived from 7-dehydrocholesterol by ultraviolet irradiation of the skin. Vitamin D3 is also found in animal food sources e.g., fatty fish (e.g., salmon, mackerel and tuna) cod liver oil, milk, etc. Vitamin D2 is found in vegetal sources like sun-exposed yeast and mushrooms. Notably, most dietary sources are not sufficiently rich in their vitamin D content.
Vitamin D (both forms D3 or D2) is a prohormone which requires two hydroxylations to finally attain its biologically active form—1,25(OH)2D. The first hydroxylation occurs in the liver, at position C25 to form 25-hydroxyvitamin D, also known as 25(OH)D or calcidiol. 25(OH)D is the major circulating form of vitamin D. The second hydroxylation occurs at position C1α to form 1,25(OH)2D, also known as calcitriol. 1,25(OH)2D is produced primarily but not exclusively in the kidneys. 1,25(OH)2D is released in blood, where it binds to vitamin D binding protein (DBP) and reaches its target tissues to exert its endocrine functions through the vitamin D receptor (VDR). 1,25(OH)2D is also produced in several extrarenal tissues for its paracrine and autocrine functions.
Indian Scenario in 2020
Recently, scientists from the Hyderabad-based National Institute of Nutrition (NIN) conducted a study on 270 apparently healthy adults (147 men and 123 women) between 30 and 70 years of age to check their vitamin levels. Blood levels of vitamins (A, B1, B2, B6, B12, folate and D) and homocysteine were assessed. Vitamin D deficiency was reported among 29% of the studied population. Metropolis hospital also reported a deficiency of Vitamin D among 81.2% of their studied pool of 14.9 Lakh samples (incl women).
“In adults, Vitamin D deficiency is associated with low bone mass and muscle weakness, which results in increased risk of fractures and bone disorders such as osteoporosis,”
Dr Srirupa Das, Medical Director, Abbott India, Mumbai (Source: India Today, August 2019)
Based on the reports of another older study published in 2014 in Nutrients (Feb6 (2)) by Ritu G, where the author shares an understanding of Vitamin D deficiency in India among men across different states.
|
State |
Incidence (%) |
Total Number of Patients Considered During Study (N) |
Level of Severity |
|
Kashmir |
76.6 |
64 |
Very High |
|
Punjab |
18.4 |
40 |
High |
|
Delhi |
18.8 |
31 |
High |
|
Uttar Pradesh |
10.9 |
Not Clear |
Not Available |
|
Tamilnadu |
23.3 |
205 |
High |
|
Maharashtra |
18.9 |
558 |
High |
|
All over India (18 cities) |
14.35 |
1525 |
High |
What is the optimal level of Vitamin D in the body?
The most reliable marker of vitamin D status is the serum concentration of 25(OH)D. vitamin D deficiency is defined as 25(OH)D < 20 ng/mL, insufficiency as 20–29 ng/mL and sufficiency as ≥30 ng/mL.
Studies reported from few developed countries show that a full body exposure to UVB radiation that results in pinkness of skin or erythemal dose is equal to an oral intake of 250–625μg (10,000–25,000 IU) of 25-hydroxy vitamin D. If one exposes 25% of the total skin, e.g. just hands, arms and face, to one erythemal dose of UVB rays can form dietary equivalent vitamin D dose of about 1,000 IU. However, there are no such calculation available for India, where the complexion of people varies from light to dark. The only reference that was available in public domain stated that the overall effect size of serum 25-OH Vitamin D level among majority of Indians is 14.16 ng/ml (study by Sandhya Selvarajan published in Indian J Endocrinol Metab. 2017)
What are the signs that you may have vitamin D deficiency?
a. You are a big time Head Sweater: “It’s one of the first, classic signs of vitamin D deficiency” as suggested by physicians.
b. As per NIH, people diagnosed with Crohn’s, celiac or inflammatory bowel disease may have a greater risk for vitamin D deficiency because of the way these gastrointestinal conditions affect fat absorption. With these and other stomach issues, fat absorption can be lower, but that in turn lowers absorption of fat-soluble vitamins like D.
c. You are 50 years or older
d. Joint pain especially in winter morning: adults have reported more achiness in bones and muscles during winter months and joints are a little more stiff when they get up in the morning. These are again some classical signals of deficiency.
What measures can be taken to check and monitor Vitamin D deficiency?
Don’t get alarmed if you blood report shows Vitamin D deficiency! Its very common in India these days and a lot has to be blamed on our lifestyle, food that we eat and other factors. However, there are ways to counter this deficiency and make up for it.
Natural Ways That Are Easy To Adopt
(A) Include Vitamin D Natural Supplements in diet
Indian diets are low in vitamin D. Oily fish like salmon and sardine and cod liver oil are some of the best sources of the vitamin D in diet. In India we have populations who prefer vegetarian food over non vegetarian and even the non-vegetarian food consists of mutton and chicken and less of sea fishes (except coastal residents). Due to intake of sea fishes, people in high latitude countries get protected from the deficiency despite the fact that they receive less sunshine. Usually men and women in high altitude countries have sun seeking behaviour coupled with the fact that their light-coloured skin quickly converts the sunlight into the nutrient. Added to this is their regular consumption of cod liver oil, which provides a whopping dose of vitamin D. Nordic people have the tradition of feeding cod liver oil to children and pregnant women as a nutritional supplement. That’s missing in India.
In India some of the quick options could be egg yolk and milk. Though it is beyond the reach for many, still this is something that the urban population must include in their daily diet. For pure vegetarians, soya milk, cheese, paneer, curd, mushrooms, cereal (oatmeals) and orange juice can be a good option.
(B) Include Vitamin D Synthetic Supplements in diet
Indian markets are flooded with multivitamin supplements which are mostly available over the counter or online. However, to avoid overdose of calcium in the body, it is always advisable to check the level of D3 in your blood and consult and registered physician. The dosage of these tablets or syrups is dependent on the individual body weight, hence self-medication is not recommended.
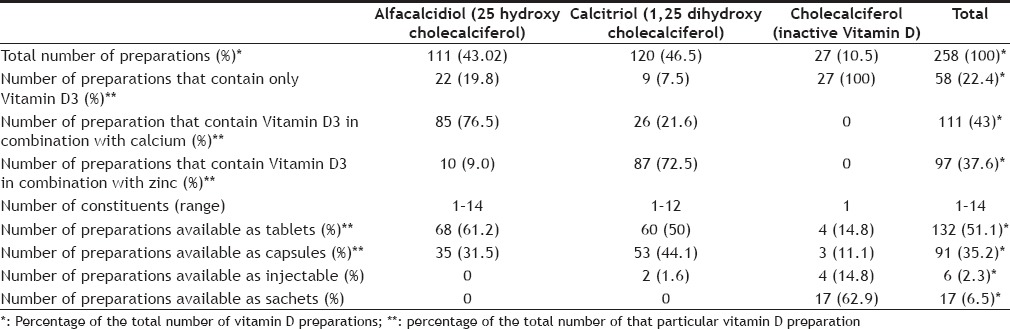
Source: Vitamin D Supplements in the Indian Market; Indian J Pharm Sci. 2016 Jan-Feb; 78(1): 41–47
(C) Yoga
Though there are no specific postures recommended for vitamin D deficiency. Surya Namaskar conducted in early hours of morning in open (sunlight) can be beneficial for overall well being.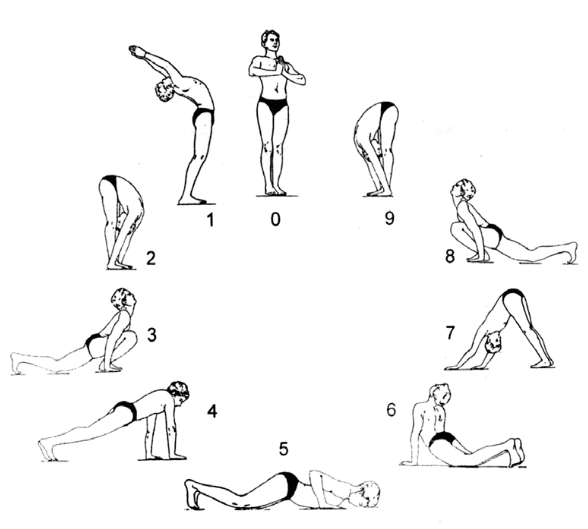
Surya Namaskar or Sun Salutation is a sequence of 12 powerful yoga poses. Its not only a great cardiovascular workout, but it is also known to have an immensely positive impact on the body and mind.
Conclusion
The skin simply doesn’t make as much vitamin D after 45+ age, and the kidneys start to grow a little less productive when it comes to converting that D into the form the body puts to good use. Hence, readers must get their vitamins level checked annually and consult physicians before switching to vitamin supplements. In general you can adopt natural vitamin D supplements in your diet and keep a healthy balance. Stay fit and stay healthy.
Key References
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3942730/
2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6060930/
3. Indian J Pharm Sci. 2016 Jan-Feb; 78(1): 41–47
4. Indian J Endocrinol Metab. 2017
- Everyone knows how to love, but only FEW know how to love forever - February 13, 2020
- A flower cannot blossom without sunshine, neither can a man live healthy without Vitamin D - January 8, 2020
- “Eat healthy, sleep well, breathe deeply, live harmoniously.” - December 30, 2019


 Please wait...
Please wait...